During controlled clinical studies conducted in the United States, 521 patients with vulvovaginal candidiasis were treated with terconazole 0.4% vaginal cream. Based on comparative analyses with placebo, the adverse experiences considered most likely related to terconazole 0.4% vaginal cream were headache (26% vs. 17% with placebo) and body pain (2.1% vs. 0% with placebo). Fever (1.7% vs. 0.5% with placebo) and chills (0.4% vs, 0% with placebo), vulvovaginal burning, itching and irritation have also been reported. The adverse drug experience on terconazole most frequently causing discontinuation was vulvovaginal itching.
DESCRIPTION
Terconazole Vaginal Cream 0.4% is a white to off-white, water washable cream for intravaginal administration containing 0.4% of the antifungal agent terconazole, cis -1-[ p -[[2-(2,4-Dichlorophenyl)-2-(1 H -1,2,4-triazol-1-ylmethyl)-1,3-dioxolan-4-yl]methoxy]phenyl]-4-isopropylpiperazine, compounded in a cream base consisting of butylated hydroxyanisole, cetyl alcohol, isopropyl myristate, polysorbate 60, polysorbate 80, propylene glycol, purified water, and stearyl alcohol.
The structural formula of terconazole is as follows:
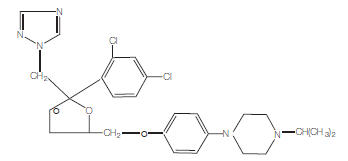 |
TERCONAZOLE C 26 H 31 CI 2 N 5 O 3 |
Terconazole, a triazole derivative, is a white to almost white powder with a molecular weight of 532.47. It is insoluble in water; sparingly soluble in ethanol; and soluble in butanol.
CLINICAL PHARMACOLOGY
Absorption
Following a single intravaginal application of a suppository containing 240 mg 14 C-terconazole to healthy women, approximately 70% (range: 64 to 76%) of terconazole remains in the vaginal area during the suppository retention period (16 hours); approximately 10% (range: 5 to 16%) of the administered radioactivity was absorbed systemically over 7 days. Maximum plasma concentrations of terconazole occur 5 to 10 hours after intravaginal application of the cream or suppository. Systemic exposure to terconazole is approximately proportional to the applied dose, whether as the cream or suppository. The rate and extent of absorption of terconazole are similar in patients with vulvovaginal candidiasis (pregnant or non-pregnant) and healthy subjects.
Distribution
Terconazole is highly protein bound (94.9%) in human plasma and the degree of binding is independent of drug concentration over the range of 0.01 to 5 mcg/mL.
Metabolism
Systemically absorbed terconazole is extensively metabolized (>95%).
Elimination
Across various studies in healthy women, after single or multiple intravaginal administration of terconazole as the cream or suppository/ovule, the mean elimination half-life of unchanged terconazole ranged from 6.4 to 8.5 hours. Following a single intravaginal administration of a suppository containing 240 mg 14 C-terconazole to hysterectomized or tubal ligated women, approximately 3 to 10% (mean ± SD: 5.7 ± 3%) of the administered radioactivity was eliminated in the urine and 2 to 6% (mean ± SD: 4.2 ± 1.6%) was eliminated in the feces during the 7-day collection period.
Multiple Dosing
There is no significant increase in maximum plasma concentration or overall exposure (AUC) after multiple daily applications of the cream for 7 days or suppositories for 3 days.
Photosensitivity reactions were observed in some normal volunteers following repeated dermal application of terconazole 2% and 0.8% creams under conditions of filtered artificial ultraviolet light.
Photosensitivity reactions have not been observed in U.S. and foreign clinical trials in patients who were treated with terconazole suppositories or vaginal cream (0.4% and 0.8%).
Microbiology
Mechanism of action
Terconazole, an azole antifungal agent, inhibits fungal cytochrome P-450-mediated 14 alpha-lanosterol demethylase enzyme. This enzyme functions to convert lanosterol to ergosterol. The accumulation of 14 alpha-methyl sterols correlates with the subsequent loss of ergosterol in the fungal cell wall and may be responsible for the antifungal activity of terconazole. Mammalian cell demethylation is less sensitive to terconazole inhibition.
Activity in vitro
Terconazole exhibits antifungal activity in vitro against Candida albicans and other Candida species. The MIC values of terconazole against most Lactobacillus spp. typically found in the human vagina were ≥ 128 mcg/mL; therefore these beneficial bacteria are not affected by drug treatment.
INDICATIONS AND USAGE
Terconazole vaginal cream is indicated for the local treatment of vulvovaginal candidiasis (moniliasis). As terconazole vaginal cream is effective only for vulvovaginitis caused by the genus Candida , the diagnosis should be confirmed by KOH smears and/or cultures.
CONTRAINDICATIONS
Patients known to be hypersensitive to terconazole or to any of the components of the cream.
WARNINGS
Anaphylaxis and toxic epidermal necrolysis have been reported during terconazole therapy. Terconazole therapy should be discontinued if anaphylaxis or toxic epidermal necrolysis develops.
PRECAUTIONS
General
For vulvovaginal use only. Terconazole is not for ophthalmic or oral use. Discontinue use and do not retreat with terconazole if sensitization, irritation, fever, chills or flu-like symptoms are reported during use.
Laboratory Tests
If there is lack of response to terconazole, appropriate microbiologic studies (standard KOH smear and/or cultures) should be repeated to confirm the diagnosis and rule out other pathogens.
Drug Interactions
The therapeutic effect of terconazole is not affected by oral contraceptive usage.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Studies to determine the carcinogenic potential of terconazole have not been performed.
Mutagenicity
Terconazole was not mutagenic when tested in vitro for induction of microbial point mutations (Ames test), or for inducing cellular transformation, or in vivo for chromosome breaks (micronucleus test) or dominant lethal mutations in mouse germ cells.
Impairment of Fertility
No impairment of fertility occurred when female rats were administered terconazole orally up to 40 mg/kg/day for a three month period.
Pregnancy
Teratogenic Effects
Pregnancy Category C
There was no evidence of teratogenicity when terconazole was administered orally up to 40 mg/kg/day (100× the recommended intravaginal human dose of the 0.4% vaginal cream formulation) in rats, or 20 mg/kg/day in rabbits, or subcutaneously up to 20 mg/kg/day in rats.
Dosages at or below 10 mg/kg/day produced no embryotoxicity; however, there was a delay in fetal ossification at 10 mg/kg/day in rats. There was some evidence of embryotoxicity in rabbits and rats at 20 to 40 mg/kg. In rats, this was reflected as a decrease in litter size and number of viable young and reduced fetal weight. There was also delay in ossification and an increased incidence of skeletal variants.
The no-effect dose of 10 mg/kg/day resulted in a mean peak plasma level of terconazole in pregnant rats of 0.176 mcg/mL which exceeds by 44 times the mean peak plasma level (0.004 mcg/mL) seen in normal subjects after intravaginal administration of terconazole 0.4% vaginal cream. This safety assessment does not account for possible exposure of the fetus through direct transfer to terconazole from the irritated vagina by diffusion across amniotic membranes.
Since terconazole is absorbed from the human vagina, it should not be used in the first trimester of pregnancy unless the physician considers it essential to the welfare of the patient.
Terconazole may be used during the second and third trimester if the potential benefit outweighs the possible risks to the fetus.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Animal studies have shown that rat offspring exposed via the milk of treated (40 mg/kg/orally) dams showed decreased survival during the first few post-partum days, but overall pup weight and weight gain were comparable to or greater than controls throughout lactation. Because many drugs are excreted in human milk, and because of the potential for adverse reaction in nursing infants from terconazole, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and efficacy in children have not been established.
Geriatric Use
Clinical studies of terconazole did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
ADVERSE REACTIONS
Adverse Reactions from Clinical Trials
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
During controlled clinical studies conducted in the United States, 521 patients with vulvovaginal candidiasis were treated with terconazole 0.4% vaginal cream. Based on comparative analyses with placebo, the adverse experiences considered most likely related to terconazole 0.4% vaginal cream were headache (26% vs. 17% with placebo) and body pain (2.1% vs. 0% with placebo). Fever (1.7% vs. 0.5% with placebo) and chills (0.4% vs, 0% with placebo), vulvovaginal burning, itching and irritation have also been reported. The adverse drug experience on terconazole most frequently causing discontinuation was vulvovaginal itching.
Post-marketing Experience
The following adverse drug reactions have been first identified during post-marketing experience with terconazole:. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General: Asthenia, Influenza-Like Illness consisting of multiple listed reactions including fever and chills, nausea, vomiting, myalgia, arthralgia, malaise
Immune: Hypersensitivity, Anaphylaxis, Face Edema
Skin: Rash, Toxic Epidermal Necrolysis, Urticaria
OVERDOSAGE
In the rat, the oral LD 50 values were found to be 1741 and 849 mg/kg for the male and female, respectively. The oral LD 50 values for the male and female dog were ≅1280 and ≥640 mg/kg, respectively.
In the event of oral ingestion of suppository or cream, supportive and symptomatic measures should be carried out. If the cream is accidentally applied to the eyes, wash with clean water or saline and seek medical attention if symptoms persist.
DOSAGE AND ADMINISTRATION
One full applicator (5 grams) of terconazole vaginal cream (20 mg terconazole) should be administered intravaginally once daily at bedtime for seven consecutive days.
Before prescribing another course of therapy, the diagnosis should be reconfirmed by smears and/or cultures and other pathogens commonly associated with vulvovaginitis ruled out. The therapeutic effect of terconazole vaginal cream is not affected by menstruation.
HOW SUPPLIED
Terconazole Vaginal Cream 0.4% is available in 45 gram (NDC 51672-1304-6) tubes with a measured-dose applicator.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Mfd. by: Taro Pharmaceuticals Inc., Brampton, Ontario, Canada L6T 1C1
Dist. by: Taro Pharmaceuticals U.S.A., Inc., Hawthorne, NY 10532
Revised: October, 2019
PK-3491-5 54
Terconazole
Vaginal Cream 0.4%
FILLING THE APPLICATOR:
1. Remove the cap from the tube.

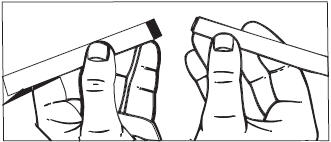
2. Use the pointed tip on the top of the cap to puncture the seal on the tube.

3. Screw the applicator onto the tube.
4. Squeeze the tube from the bottom and fill the applicator until the plunger stops. DO NOT release pressure on the tube until you have separated it from the filled applicator.
5. Unscrew the applicator from the tube. After each use, replace the cap and roll up the tube from the bottom.

USING THE APPLICATOR:
1. Lie on your back with your knees drawn up toward your chest.
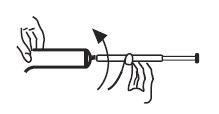
2. Holding the applicator by the ribbed end of the barrel, insert the filled applicator into the vagina as far as it will comfortably go.
3. Slowly press the plunger of the applicator to release the cream into the vagina.

4. Remove the applicator from the vagina.
5. Apply one applicatorful each night for as many days at bedtime, as directed by your doctor.
CLEANING THE APPLICATOR:
After each use, you should thoroughly clean the applicator by following the procedure below:
1. Pull the plunger out of the barrel.
2. Wash the pieces with lukewarm, soapy water, and dry them thoroughly.
3. Put the applicator back together by gently pushing the plunger into the barrel as far as it will go.
NOTE: Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. See end flap of carton or crimp of tube for lot number and expiration date.
A WORD ABOUT YEAST INFECTIONS
Why do yeast infections occur?
Yeast infections are caused by an organism called Candida (KAN di duh). It may be present in small and harmless amounts in the mouth, digestive tract, and vagina. Sometimes the natural balance of the vagina becomes upset. This may lead to rapid growth of Candida, which results in a yeast infection. Symptoms of a yeast infection include itching, burning, redness, and an abnormal discharge.
Your doctor can make the diagnosis of a yeast infection by evaluating your symptoms and looking at a sample of the discharge under the microscope.
How can I prevent yeast infections?
Certain factors may increase your chance of developing a yeast infection. These factors don’t actually cause the problem, but they may create a situation that allows the yeast to grow rapidly.
- Clothing: Tight jeans, nylon underwear, pantyhose, and wet bathing suits can hold in heat and moisture (two conditions in which yeast organisms thrive). Looser pants or skirts, 100% cotton underwear, and stockings may help avoid this problem.
- Diet: Cutting down on sweets, milk products, and artificial sweeteners may reduce the risk of yeast infections.
- Antibiotics: Antibiotics work by eliminating disease-causing organisms. While they are helpful in curing other problems, antibiotics may lead to an overgrowth of Candida in the vagina.
- Pregnancy: Hormonal changes in the body during pregnancy encourage the growth of yeast. This is a very common time for an infection to occur. Until the baby is born, it may be hard to completely eliminate yeast infections. If you believe you are pregnant, tell your doctor.
- Menstruation: Sometimes monthly changes in hormone levels may lead to yeast infections.
- Diabetes: In addition to heat and moisture, yeast thrives on sugar. Because diabetics often have sugar in their urine, their vaginas are rich in this substance. Careful control of diabetes may help prevent yeast infection.
Controlling these factors can help eliminate yeast infections and may prevent them from coming back.
Some other helpful tips:
1. For best results, be sure to use the medication as prescribed by your doctor, even if you feel better quickly.
2. Avoid sexual intercourse, if your doctor advises you to do so.
3. If your partner has any penile itching, redness, or discomfort, he should consult his physician and mention that you are being treated for a yeast infection.
4. You can use the medication even if you are having your menstrual period. However, you should not use tampons because they may absorb the medication. Instead, use external pads or napkins until you have finished your medication. You may also wish to wear a sanitary napkin if the vaginal medication leaks.
5. Dry the genital area thoroughly after showering, bathing, or swimming. Change out of a wet bathing suit or damp exercise clothes as soon as possible. A dry environment is less likely to encourage the growth of yeast.
6. Wipe from front to rear (away from the vagina) after a bowel movement.
7. Don’t douche unless your doctor specifically tells you to do so. Douching may disturb the vaginal balance.
8. Don’t scratch if you can help it. Scratching can cause more irritation and spread the infection.
9. Discuss with your physician any medication you are already taking. Certain types of medication can make your vagina more susceptible to infection.
10. Eat nutritious meals to promote your general health.
Mfd. by:
Taro Pharmaceuticals Inc.
Brampton, Ontario, Canada L6T 1C1
Dist. by:
Taro Pharmaceuticals U.S.A., Inc.
Hawthorne, NY 10532
Revised: October, 2019
PK-3491-5 54
PRINCIPAL DISPLAY PANEL – 45 g Tube Carton
TUBE AND APPLICATOR
FOR VAGINAL USE ONLY.
Keep this and all medications out of the reach of children.
DESCRIPTION
Terconazole vaginal cream 0.4% is a white to off-white, water washable cream for intravaginal administration containing 0.4% of the antifungal agent terconazole, cis -1-[ p -[[2-(2,4-Dichlorophenyl)-2-(1 H -1,2,4-triazol-1-ylmethyl)-1,3-dioxolan-4-yl]methoxy]phenyl]-4-isopropylpiperazine, compounded in a cream base consisting of butylated hydroxyanisole, cetyl alcohol, isopropyl myristate, polysorbate 60, polysorbate 80, propylene glycol, stearyl alcohol, and purified water.
The structural formula of terconazole is as follows:

Terconazole, a triazole derivative, is a white to almost white powder with a molecular weight of 532.47. It is insoluble in water; sparingly soluble in ethanol; and soluble in butanol.
CLINICAL PHARMACOLOGY
Following a single intravaginal application of a suppository containing 240 mg 14 C-terconazole to healthy women, approximately 70% (range: 64 to 76%) of terconazole remains in the vaginal area during the suppository retention period (16 hours); approximately 10% (range: 5 to 16%) of the administered radioactivity was absorbed systemically over 7 days. Maximum plasma concentrations of terconazole occur 5 to 10 hours after intravaginal application of the cream or suppository. Systemic exposure to terconazole is approximately proportional to the applied dose, whether as the cream or suppository. The rate and extent of absorption of terconazole are similar in patients with vulvovaginal candidiasis (pregnant or non-pregnant) and healthy subjects.
Terconazole is highly protein bound (94.9%) in human plasma and the degree of binding is independent of drug concentration over the range of 0.01 to 5 mcg/mL.
Systemically absorbed terconazole is extensively metabolized (>95%).
Across various studies in healthy women, after single or multiple intravaginal administration of terconazole as the cream or suppository/ovule, the mean elimination half-life of unchanged terconazole ranged from 6.4 to 8.5 hours. Following a single intravaginal administration of a suppository containing 240 mg 14 C-terconazole to hysterectomized or tubal ligated women, approximately 3 to 10% (mean ±SD: 5.7 ± 3%) of the administered radioactivity was eliminated in the urine and 2 to 6% (mean ± SD: 4.2 ± 1.6%) was eliminated in the feces during the 7-day collection period.
There is no significant increase in maximum plasma concentration or overall exposure (AUC) after multiple daily applications of the cream for 7 days or suppositories for 3 days.
Photosensitivity reactions have not been observed in U.S. and foreign clinical trials in patients who were treated with terconazole vaginal cream (0.4%).
Mechanism of action
Terconazole, an azole antifungal agent, inhibits fungal cytochrome P-450-mediated 14 alpha-lanosterol demethylase enzyme. This enzyme functions to convert lanosterol to ergosterol. The accumulation of 14 alpha-methyl sterols correlates with the subsequent loss of ergosterol in the fungal cell wall and may be responsible for the antifungal activity of terconazole. Mammalian cell demethylation is less sensitive to terconazole inhibition.
Activity in vitro
Terconazole exhibits antifungal activity in vitro against Candida albicans and other Candida species. The MIC values of terconazole against most Lactobacillus spp. typically found in the human vagina were ≥ 128 mcg/mL; therefore these beneficial bacteria are not affected by drug treatment.
INDICATIONS AND USAGE
Terconazole vaginal cream 0.4% is indicated for the local treatment of vulvovaginal candidiasis (moniliasis). As terconazole vaginal cream 0.4% is effective only for vulvovaginitis caused by the genus Candida , the diagnosis should be confirmed by KOH smears and/or cultures.
CONTRAINDICATIONS
Patients known to be hypersensitive to terconazole or to any of the components of the cream.
WARNINGS
Anaphylaxis and toxic epidermal necrolysis have been reported during terconazole therapy. Terconazole therapy should be discontinued if anaphylaxis or toxic epidermal necrolysis develops.
PRECAUTIONS
For vaginal use only. Terconazole Vaginal Cream 0.4% is not for ophthalmic or oral use. Discontinue use and do not retreat with terconazole if sensitization, irritation, fever, chills or flu-like symptoms are reported during use.
If there is a lack of response to terconazole, appropriate microbiologic studies (standard KOH smear and/or cultures) should be repeated to confirm the diagnosis and rule out other pathogens.
The therapeutic effect of terconazole is not affected by oral contraceptive usage.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies to determine the carcinogenic potential of terconazole have not been performed.
Terconazole was not mutagenic when tested in vitro for induction of microbial point mutations (Ames test), or for inducing cellular transformation, or in vivo for chromosome breaks (micronucleus test) or dominant lethal mutations in mouse germ cells.
Impairment of Fertility
No impairment of fertility occurred when female rats were administered terconazole orally up to 40 mg/kg/day for a three month period.
Teratogenic Effects, Pregnancy Category C:
There was no evidence of teratogenicity when terconazole was administered orally up to 40 mg/kg/day (100x the intravaginal human dose of the 0.4% vaginal cream formulation) in rats, or 20 mg/kg/day in rabbits, or subcutaneously up to 20 mg/kg/day in rats.
Dosages at or below 10 mg/kg/day produced no embryotoxicity; however, there was a delay in fetal ossification at 10 mg/kg/day in rats. There was some evidence of embryotoxicity in rabbits and rats at 20 to 40 mg/kg. In rats, this was reflected as a decrease in litter size and number of viable young and reduced fetal weight. There was also delay in ossification and an increase incidence of skeletal variants.
The no-effect dose of 10 mg/kg/day resulted in a mean peak plasma level of terconazole in pregnant rats of 0.176 mcg/mL which exceeds by 44 times the mean peak plasma level (0.004 mcg/mL) seen in normal subjects after intravaginal administration of terconazole vaginal cream 0.4%. This safety assessment does not account for possible exposure of the fetus through direct transfer to terconazole from the irritated vagina by diffusion across amniotic membranes.
Since terconazole is absorbed from the human vagina, it should not be used in the first trimester of pregnancy unless the physician considers it essential to the welfare of the patient.
Terconazole may be used during the second and third trimester if the potential benefit outweighs the possible risks to the fetus.
It is not known whether this drug is excreted in human milk. Animal studies have shown that rat offspring exposed via the milk of treated (40 mg/kg/orally) dams showed decreased survival during the first few post-partum days, but overall pup weight and weight gain were comparable to or greater than controls throughout lactation. Because many drugs are excreted in human milk, and because of the potential for adverse reaction in nursing infants from terconazole, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Safety and efficacy in children have not been established.
Clinical studies of terconazole vaginal cream did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
ADVERSE REACTIONS
Adverse Reactions from Clinical Trials
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
During controlled clinical studies conducted in the United States, 521 patients with vulvovaginal candidiasis were treated with terconazole 0.4% vaginal cream. Based on comparative analyses with placebo, the adverse experiences considered most likely related to terconazole 0.4% vaginal cream were headache (26% vs. 17% with placebo) and body pain (2.1% vs. 0% with placebo). Fever (1.7% vs. 0.5% with placebo) and chills (0.4% vs. 0.0% with placebo), vulvovaginal burning, itching and irritation have also been reported. The adverse drug experience on terconazole most frequently causing discontinuation was vulvovaginal itching.
The following adverse drug reactions have been first identified during post-marketing experience with terconazole vaginal cream 0.4%. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General: Asthenia, Influenza-Like Illness consisting of multiple listed reactions including fever and chills, nausea, vomiting, myalgia, arthralgia, malaise
Immune: Hypersensitivity, Anaphylaxis, Face Edema
Skin: Rash, Toxic Epidermal Necrolysis, Urticaria
OVERDOSAGE
In the rat, the oral LD 50 values were found to be 1741 and 849 mg/kg for the male and female, respectively. The oral LD 50 values for the male and female dog were ≅1280 and ≥640 mg/kg, respectively.
In the event of oral ingestion of the cream, supportive and symptomatic measures should be carried out. If the cream is accidentally applied to the eyes, wash with clean water or saline and seek medical attention if symptoms persist.
DOSAGE AND ADMINISTRATION
One full applicator (5 g) of terconazole vaginal cream 0.4% (20 mg terconazole) should be administered intravaginally once daily at bedtime for seven consecutive days.
Before prescribing another course of therapy, the diagnosis should be reconfirmed by smears and/or cultures and other pathogens commonly associated with vulvovaginitis ruled out. The therapeutic effect of terconazole vaginal cream 0.4% is not affected by menstruation.
HOW SUPPLIED
Terconazole Vaginal Cream 0.4% is available in:
NDC 0168-0346-46 45 gram tube, with a measured dose applicator.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
E. FOUGERA & CO.
A division of
Fougera
PHARMACEUTICALS INC.
Melville, New York 11747
Terconazole Vaginal Cream 0.4%
PATIENT INSTRUCTIONS
Filling the applicator:
1. Remove the cap from the tube. 2. Use the pointed tip on the top of the cap to puncture the seal on the tube.

3. Screw the applicator onto the tube.
4. Squeeze the tube from the bottom and fill the applicator until the plunger stops. 5. Unscrew the applicator from the tube.
Using the applicator:
1. Lie on your back with your knees drawn up toward your chest. 2. Holding the applicator by the ribbed end of the barrel, insert the filled applicator into the vagina as far as it will comfortably go .

3. Slowly press the plunger of the applicator to release the cream into the vagina. 4. Remove the applicator from the vagina. 5. Apply one applicatorful each night for as many days at bedtime, as directed by your doctor.
Cleaning the applicator: After each use, you should thoroughly clean the applicator by following the procedure below:
1. Pull the plunger out of the barrel. 2. Wash both pieces with lukewarm, soapy water, and dry them thoroughly. 3. Put the applicator back together by gently pushing the plunger into the barrel as far as it will go.
NOTE: Store at 20° to 25°C (68° to 77°F)
[see USP Controlled Room Temperature].
See side flap of carton for lot number and expiration date.
A WORD ABOUT YEAST INFECTIONS
Why do yeast infections occur?
Yeast infections are caused by an organism called Candida (KAN di duh). It may be present in small and harmless amounts in the mouth, digestive tract, and vagina. Sometimes the natural balance of the vagina becomes upset. This may lead to rapid growth of Candida, which results in a yeast infection. Symptoms of a yeast infection include itching, burning, redness, and an abnormal discharge.
Your doctor can make the diagnosis of a yeast infection by evaluating your symptoms and looking at a sample of the discharge under the microscope.
How can I prevent yeast infections?
Certain factors may increase your chance of developing a yeast infection. These factors don’t actually cause the problem, but they may create a situation that allows the yeast to grow rapidly.
• Clothing: Tight jeans, nylon underwear, pantyhose, and wet bathing suits can hold in heat and moisture (two conditions in which yeast organisms thrive). Looser pants or skirts, 100% cotton underwear, and stockings may help avoid this problem. • Diet: Cutting down on sweets, milk products, and artificial sweeteners may reduce the risk of yeast infections. • Antibiotics: Antibiotics work by eliminating disease-causing organisms. While they are helpful in curing other problems, antibiotics may lead to an overgrowth of Candida in the vagina. • Pregnancy: Hormonal changes in the body during pregnancy encourage the growth of yeast. This is a very common time for an infection to occur. Until the baby is born, it may be hard to completely eliminate yeast infections. If you believe you are pregnant, tell your doctor. • Menstruation: Sometimes monthly changes in hormone levels may lead to yeast infections. • Diabetes: In addition to heat and moisture, yeast thrives on sugar. Because diabetics often have sugar in their urine, their vaginas are rich in this substance. Careful control of diabetes may help prevent yeast infections.
Controlling these factors can help eliminate yeast infections and may prevent them from coming back.
Some other helpful tips:
1. For best results, be sure to use the medication as prescribed by your doctor, even if you feel better very quickly. 2. Avoid sexual intercourse, if your doctor advises you to do so. 3. If your partner has any penile itching, redness, or discomfort, he should consult his physician and mention that you are being treated for a yeast infection. 4. You can use the medication even if you are having your menstrual period. However, you should not use tampons because they may absorb the medication. Instead, use external pads or napkins until you have finished your medication. You may also wish to wear a sanitary napkin if the vaginal medication leaks. 5. Dry the genital area thoroughly after showering, bathing, or swimming. Change out of a wet bathing suit or damp exercise clothes as soon as possible. A dry environment is less likely to encourage the growth of yeast. 6. Wipe from front to rear (away from the vagina) after a bowel movement. 7. Don’t douche unless your doctor specifically tells you to do so. Douching may disturb the vaginal balance. 8. Don’t scratch if you can help it. Scratching can cause more irritation and spread the infection. 9. Discuss with your physician any medication you are already taking. Certain types of medication can make your vagina more susceptible to infection. 10. Eat nutritious meals to promote your general health.
KEEP OUT OF THE REACH OF CHILDREN.
E. FOUGERA & CO.
A division of
Fougera
PHARMACEUTICALS INC.
Melville, New York 11747
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – 45 GRAM TUBE
TERCONAZOLE
VAGINAL CREAM
0.4%






