10) SPL / Science Source
What’s Causing This Pain in the Back of My Knee?
You may feel pain in the back of the knee after an injury or due to another health condition, such as a cyst or arthritis. More rarely, it can be an indicator of a more serious condition like a blood clot.

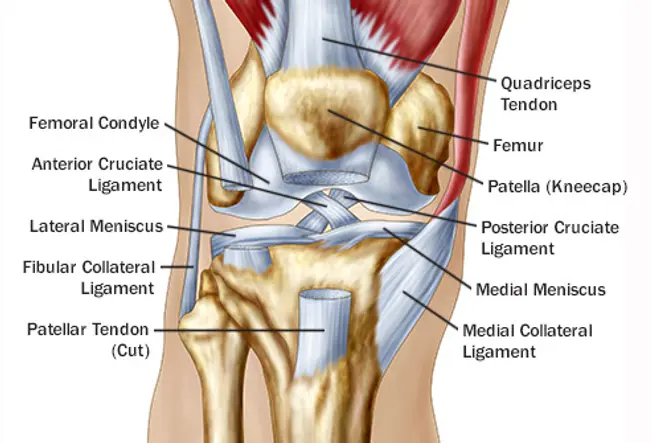
The knee is your body’s biggest joint and one of its most injury-prone areas. It’s made up of bones that can fracture or move out of joint, as well as cartilage, ligaments, and tendons that can strain or tear.
Some knee injuries eventually heal on their own with rest and care. Others require surgery or other medical interventions. Sometimes pain is a sign of a chronic condition like arthritis that damages the knee gradually over time.
Here are some of the conditions that can cause pain in the back of your knee, and what to expect if you have one of them.
A cramp is a tightening of a muscle. Muscles in the calves are most likely to cramp, but other leg muscles can cramp up, too — including muscles in the back of the thigh near the knee.
You’re more likely to have leg cramps when you exercise or during pregnancy. Other possible causes include:
- nerve problems in your legs
- dehydration
- infections, such as tetanus
- toxins, like lead or mercury in the blood
- liver disease
When you have a cramp, you’ll suddenly feel your muscle contract, or spasm. The pain lasts anywhere from a few seconds to 10 minutes. After the cramp passes, the muscle may be sore for a few hours. Here’s how to put a stop to the pain and prevent future leg cramps.
Jumper’s knee is an injury to the tendon — the cord that connects your kneecap (patella) to your shinbone. It’s also called patellar tendonitis. It can happen when you jump or change direction, such as when playing volleyball or basketball.
These movements can cause tiny tears in the tendon. Eventually, the tendon swells up and weakens.
Jumper’s knee causes pain below the kneecap. The pain gets worse over time. Other symptoms include:
- weakness
- stiffness
- trouble bending and straightening your knee
The hamstring consists of a trio of muscles that run down the back of your thigh:
- semitendinosus muscle
- semimembranosus muscle
- biceps femoris muscle
These muscles allow you to bend your knee.
Injuring one of these muscles is called a pulled hamstring or a hamstring strain. A hamstring strain happens when the muscle is stretched too far. The muscle can completely tear, which can take months to heal.
When you injure your hamstring muscle, you’ll feel a sudden pain. Injuries to the biceps femoris — called biceps femoris tendinopathy — cause pain in the back of the knee.
Other symptoms include:
- swelling
- bruising
- weakness in the back of your leg
This type of injury is common in athletes who run fast in sports like soccer, basketball, tennis, or track. Stretching the muscles out before play can help prevent this injury from occurring.
A Baker’s cyst is a fluid-filled sac that forms behind the knee. The fluid inside the cyst is synovial fluid. Normally, this fluid acts as a lubricant for your knee joint. But if you have arthritis or a knee injury, your knee may produce too much synovial fluid. The extra fluid can build up and form a cyst.
- pain in and behind your knee
- swelling behind your knee
- stiffness and trouble flexing your knee
These symptoms can get worse when you’re active. If the cyst bursts, you’ll feel a sharp pain in your knee.
Baker’s cysts sometimes go away on their own. To treat a large or painful cyst, you may need steroid injections, physical therapy, or to have the cyst drained. It’s important to determine if an underlying problem is causing the cyst, such as arthritis. If so, taking care of this problem first may result in the Baker’s cyst clearing up.
The gastrocnemius muscle and the soleus muscle make up your calf, which is the back of your lower leg. These muscles help you bend your knee and point your toes.
Any sport that requires you to quickly go from a standing position to a run — like tennis or squash — can strain or tear the gastrocnemius muscle. You’ll know that you’ve strained this muscle by the sudden pain it causes in the back of your leg.
Other symptoms include:
- pain and swelling in the calf
- bruising in the calf
- trouble standing on tiptoe
The pain should subside depending on the size of the tear. Resting, elevating the leg, and icing the injured area will help it heal faster.
The meniscus is a wedge-shaped piece of cartilage that cushions and stabilizes your knee joint. Each of your knees has two menisci — one on either side of the knee.
Athletes sometimes tear the meniscus when they squat and twist the knee. As you get older, your meniscus weakens and degenerates and is more likely to tear with any twisting motion.
When you tear a meniscus, you might hear a “popping” sound. At first the injury might not hurt. But after you walk on it for a few days, the knee can become more painful.
Other symptoms of a meniscus tear are:
- stiffness in the knee
- swelling
- weakness
- locking or giving way of the knee
Rest, ice, and elevation of the affected knee can help alleviate the symptoms and allow it to heal faster. If the tear doesn’t improve on its own, you might need surgery to repair it.
The anterior cruciate ligament (ACL) is a band of tissue that runs through the front of your knee joint. It connects your thighbone to your shinbone and helps stabilize and provide movement to your knee.
Most ACL injuries happen when you slow down, stop, or change direction suddenly while running. You can also strain or tear this ligament if you land a jump wrong, or you get hit in a contact sport like football.
You might feel a “pop” when the injury happens. Afterward, your knee will hurt and swell up. You might have trouble fully moving your knee and feel pain when you walk.
Rest and physical therapy can help an ACL strain heal. If the ligament is torn, you’ll often need surgery to fix it. Here’s what to expect during ACL reconstruction.
The posterior cruciate ligament (PCL) is the ACL’s partner. It’s another band of tissue that connects your thighbone to your shinbone and supports your knee. However, the PCL isn’t as likely to get injured as the ACL.
You can injure the PCL if you take a hard blow to the front of your knee, such as in a car accident. Sometimes injuries occur from twisting the knee or missing a step while walking.
Stretching the ligament too far causes a strain. With enough pressure, the ligament can tear into two parts.
Along with pain, a PCL injury causes:
- swelling of the knee
- stiffness
- trouble walking
- weakness of the knee
Rest, ice, and elevation can help a PCL injury heal faster. You might need surgery if you’ve injured more than one ligament in your knee, have symptoms of instability, or you also have cartilage damage.
Why Knees Hurt
Your knees have lots of moving parts, and you use them a lot, so lots of things can go wrong. Too much of one kind of motion, especially if you don’t work up to it, can lead to “overuse” injuries. Simple wear and tear is a problem, especially as you age. Accidents can crack bones and tear tissue. With some conditions, your body attacks its own joints. Your doctor can help you sort out what’s going on with your knee when it doesn’t feel right.

Dislocations and Fractures
2/15
If your knee hurts intensely after a bump, bang, or fall, you may have broken one of the bones that meet up there — the thigh, shin, and kneecap — or shifted one out of place. Go to the emergency room or see a doctor as soon as possible. Sometimes fractures happen more slowly, causing tiny cracks at the ends of the leg bones. This can happen when you’ve started using your knee more.

Torn Anterior Cruciate Ligament
3/15
You hear a pop and can’t move after you suddenly change direction — often while playing soccer, football, or basketball. You may have torn your ACL, which connects the femur and the tibia and prevents the tibia from moving too far forward. Your knee will hurt and swell and feel unstable.
You can tear or strain any of the tissues that hold your knee together: Ligaments connect bones to each other; tendons connect muscle to bone. Irritated tendons from using them too much? That’s tendinitis.
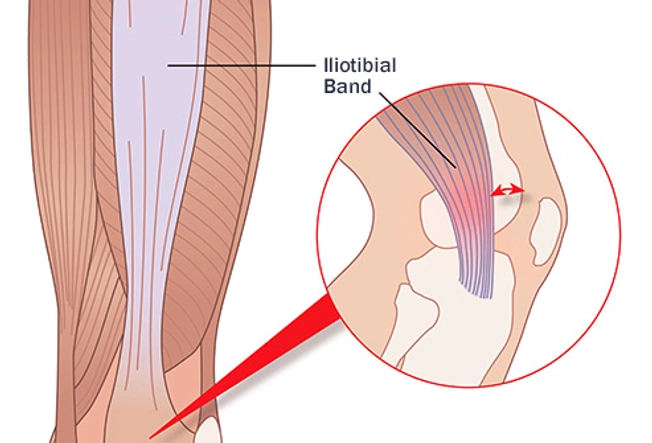
Iliotibial Band Syndrome
4/15
The “IT band,” a ligament that runs along the outside of your thigh, can rub against the bone and get irritated and swollen. You’re more likely to get this when you run or ride your bike for exercise. It might hurt more if you go downhill or sit for a while. You may feel better after you warm up, but if you don’t rest the injury and give it a chance to heal, it could get worse.

Osteoarthritis
5/15
It’s tough to bend or stretch your leg. Your knee feels stiff and sore and may swell after you’ve been moving around. You’ve probably worn down the cartilage, the stuff that helps cushion the ends of your bones. Because that takes time, this kind of arthritis is more common in people 65 and older. If you’re younger, you may get it because you’ve used your knee a lot after an injury, like a ligament tear.
Inflammatory Arthritis
6/15
Besides pain and swelling, you may also feel tired, sick, or feverish. When you have an autoimmune disease, your immune system, which is meant to fight off germs, may attack your knees. For example, rheumatoid arthritis tends to affect hands and other joints in pairs on both sides of the body. Lupus goes after joints, muscles, and organs all over. Psoriatic arthritis often causes thick, discolored patches of skin, along with joint pain.

Bursitis
7/15
This makes your knee swollen, stiff, and warm or tender to the touch, usually because you’ve overworked it. The condition is also known as “housemaid’s knee” or “clergyman’s knee” because people with these jobs are kneeling so much. It happens when small, fluid-filled sacs called bursa that help cushion your knee joint get irritated and swollen. You may ache even when you’re resting.

Runner’s Knee
8/15
You’ll feel this in the front of your knee, around the kneecap. Your knee may hurt after you sit with it bent for a while or when you try to kneel. It may pop or crack when you climb stairs. Typically, patellofemoral pain syndrome comes from overuse, misalignment between your hip and ankle, a weak thigh muscle, or the breakdown of cartilage behind your kneecap — or a combination of these. It’s common in women and young athletes.

Torn Meniscus
9/15
A sudden twist or pivot — especially with your full weight on your knee — can tear a meniscus, the rubbery cartilage that acts as a cushion between the bones of your thigh and shin. You have one on each side of your ACL. They may be more susceptible to tears because of arthritis or age. The pain can be hard to pinpoint and describe. Your knee may get stiff, swollen, and hard to move and extend.

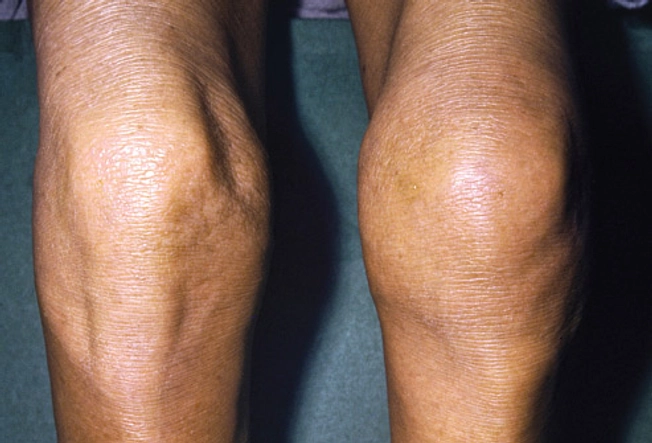
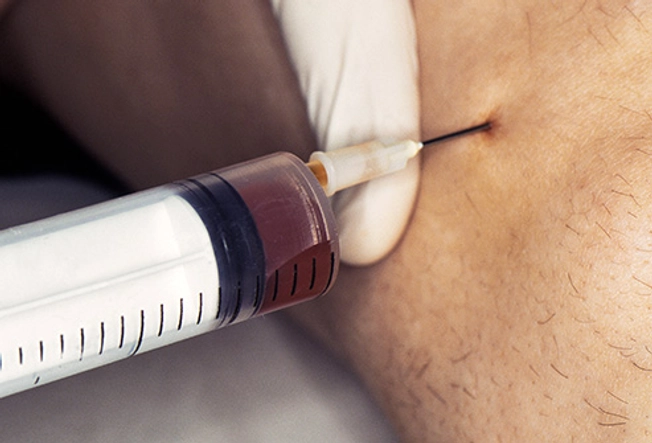
Baker’s Cyst (Popliteal Cyst)
10/15
This fluid-filled sac at the back of your knee may bulge out or get so tight that it’s hard to fully bend or stretch your leg. It may be caused by another problem, like arthritis or a tear in your meniscus. The cyst itself usually doesn’t hurt unless it bursts, which can make the back of your knee and calf swell and bruise.
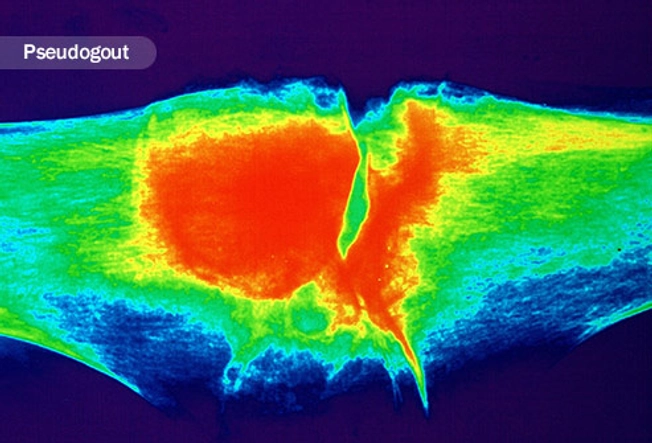
Gout and Pseudogout
11/15
Both have similar symptoms: The pain and swelling are often intense and hit you fast. Your knee may be stiff, red, and hot. It happens when crystals gather in the joint. Gout is from a buildup of uric acid and often affects the big toe. Pseudogout is caused by calcium pyrophosphate.
Infection
12/15
Another illness or a direct injury to the joint can cause septic arthritis. The pain will come on quickly, and you’ll also be sick, cranky, and running a fever. Your doctor may use a needle to take some fluid from your knee to figure out which bacteria is causing it so they know how to treat it. Though it doesn’t happen as much, viruses and parasites can infect your joints, too.

Referred Pain
13/15
Problems somewhere else — in your back, hip, or foot, for example — can make your knee sore. Nerves can move pain from one area to another, or your brain may get confused about the source of pain signals. The feeling is real, but there may be nothing wrong with your knee itself.

What You Can Do
14/15
Take over-the-counter NSAID drugs like ibuprofen and naproxen to ease pain and swelling. RICE — rest, ice, compression, and elevation — can often help, too: Get off your feet. Raise your leg so it’s higher than your heart. Put a cold pack in a thin cloth or towel on your knee for 10-20 minutes at a time, several times a day. Wrap an elastic bandage around your knee when you’re up and about, snug but not tight.

When to See Your Doctor
15/15
Don’t wait if your knee pain is sudden and intense. Pick up the phone if it won’t go away or gets worse.
To make a diagnosis, your doctor might take X-rays or other images of your knee. Blood or knee fluid samples can help confirm or rule out certain conditions. Treatment may include medication, special exercises, braces, or in some cases surgery. Losing weight could help lessen pressure and strain on your knees.
Show Sources
IMAGES PROVIDED BY:
1) Stocktrek Images / Science Source
2) (Left to right) stockdevil / Thinkstock, Steven Needell / Science Source
3) janulla / Thinkstock
4) Peter Gardiner / Science Source
5) seb_ra / Thinkstock
6) Martin Rotker / Medical Images
7) AndreyPopov / Thinkstock
8) jacoblund / Thinkstock
9) CNRI / Science Source
10) SPL / Science Source
11) Joubert / Science Source
12) Hercules Robinson / Medical Images
13) AndreyPopov / Thinkstock
14) sarmoho / Thinkstock
15) Pixel_away / Thinkstock
Mayo Clinic: “Knee pain,” “Torn meniscus,” “Baker’s cyst,” “Gout,” “Pseudogout,” “Septic arthritis.”
UpToDate: “Approach to the adult with knee pain likely of musculoskeletal origin,” “Approach to the adult with unspecified knee pain,” “Iliotibial band syndrome.”
OrthoInfo: “Common Knee Injuries,” “Patellofemoral Pain Syndrome,” “What Are NSAIDs?” “Sprains, Strains and Other Soft-Tissue Injuries.”
Arthritis Foundation: “What is Osteoarthritis?” “Benefits of Weight Loss.”
National Institute of Arthritis and Musculoskeletal and Skin Diseases: “Arthritis,” “Rheumatoid Arthritis,” “Gout” “Handout on Health: Rheumatoid Arthritis.”
CDC: “National Institute for Occupational Safety and Health: Preventing Knee Injuries and Disorders in Carpet Layers.”
Annals of The Royal College of Surgeons of England: “Hip osteoarthritis: where is the pain?”
BMJ Case Reports: “Hip arthritis presenting as knee pain.”
Medical News Today: “Knees ache? it could be your hips’ fault.”






