A clot can give you different symptoms based on where it is. A PE can give you a fast pulse, chest pain, bloody cough, and shortness of breath. Get to the hospital right away. You also might have no signs.
Blood Clot Symptoms to Know
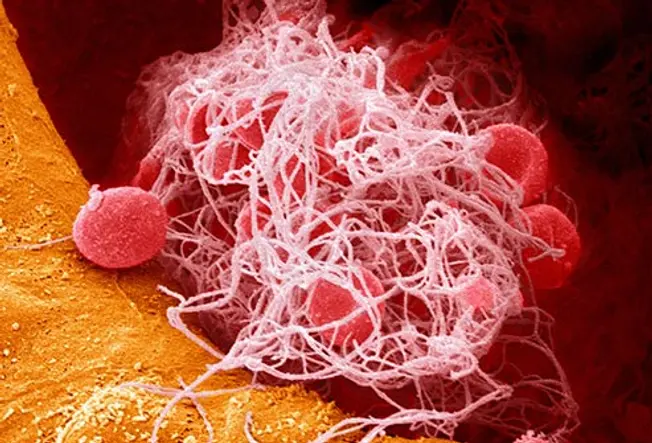
It’s a clump of cells and protein in your blood. A clot helps slow bleeding when you’re injured. It usually dissolves as you heal. But if it doesn’t, or if it forms when it’s not needed, it can clog up or completely block a blood vessel.

What Problems Can It Cause?
2/14
An unexpected clot can lead to serious problems and even death. In an artery, it can give you a heart attack or a stroke. If it happens in a vein, you can feel pain and swelling. A clot deep inside your body is called a deep vein thrombosis (DVT). One in your lungs is a pulmonary embolism (PE). They’re both medical emergencies.

Know Your Chances
3/14
You can get a blood clot if you break a bone or pull a muscle badly. But sometimes you may not know why it happened or even realize you have one. There are clues though. Your odds of a clot are higher if you:
- Are recovering from surgery or had to sit for many hours on a flight or in a wheelchair
- Are overweight or obese
- Have diabetes or high cholesterol
- Are over 60

Clue: Swelling
4/14
When a clot slows or stops the flow of blood, it can build up in the vessel and make it swell. If it happens in your lower leg or calf, it’s often a sign of DVT. But you also can have a clot in your arms or belly. Even after it goes away, one in three people still have swelling and sometimes pain and sores from damage to the blood vessel.

Clue: Skin Color
5/14
If a clot plugs up veins in your arms or legs, they may look bluish or reddish. Your skin also might stay discolored from the damage to blood vessels afterward. A PE in your lung could make your skin pale, bluish, and clammy.

Clue: Pain
6/14
Sudden, intense chest pain could mean the clot has broken off and caused a PE. Or it could be a sign that a clot in your artery gave you a heart attack. If so, you also might feel pain in your arm, especially on the left. A clot often hurts where it’s located, like in your lower leg, stomach, or under your throat.

Clue: Trouble Breathing
7/14
This is a serious symptom. It could be a sign that you have a clot in your lung or your heart. Your heart might also race, or you may feel sweaty or faint.
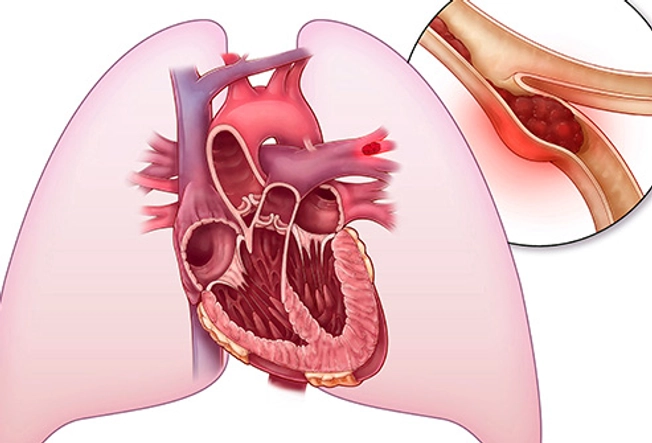
Location: Lung
8/14
A clot can give you different symptoms based on where it is. A PE can give you a fast pulse, chest pain, bloody cough, and shortness of breath. Get to the hospital right away. You also might have no signs.

Location: Heart
9/14
This can feel similar to a clot in the lung. But if it’s a heart attack, you also might feel nausea and lightheadedness along with the chest pain. Either way, call 911 or get to a hospital right away.
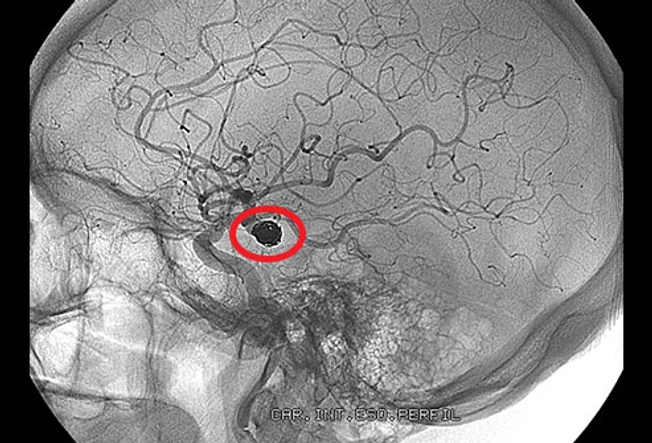
Location: Brain
10/14
Pressure builds when blood can’t flow normally. A severe blockage sometimes can lead to a stroke. Without oxygen from the blood, your brain cells start to die in minutes. A clot in your brain can cause headaches, confusion, seizures, speech problems, and weakness, sometimes on just one side of the body.

Location: Belly
11/14
Often, you have no symptoms at all. Blocked veins in the stomach or esophagus, a tube that connects it to your throat, can rip and leak blood. That can hurt a lot. You may poop or vomit blood, and your stool might look black and smell unusually bad.

Location: Kidneys
12/14
Also called renal vein thrombosis, these clots usually grow slowly and mostly in adults. You probably won’t have symptoms unless a piece breaks off and lodges in your lung. Rarely, especially in children, it can happen fast and cause nausea, fever, and vomiting. You also might have blood in your pee and go less often.

If You Suspect a Blood Clot
13/14
See your doctor or go to the emergency room right away. A clot can be deadly, and you won’t know for sure you have it until you get checked. Your doctor may give you a clot-busting drug or surgically thread a thin tube to the site of the clot to dissolve it.

Prevention Tips
14/14
You can act to lower your odds of a clot. First, keep a healthy weight, eat right, and exercise. Also:
- Don’t sit or stay still for long, especially after a long trip or surgery.
- If you’re a desk jockey, get up and move at least every couple of hours. Flex your legs, feet, and toes in your chair.
- Check if tight-fitting compression socks or garments can help your blood flow.
- Ask your doctor if you might need to take clot-fighting drugs called anticoagulants.
Show Sources
IMAGES PROVIDED BY:
- Science Source
- Getty Images
- Getty Images
- Science Source
- Thinkstock
- Getty Images
- Thinkstock
- Science Source
- Thinkstock
- Thinkstock
- Thinkstock
- Thinkstock
- Thinkstock
- Thinkstock
AARP: “Blood Clots: Are You at Risk?”
ACP Hospitalist: “Splanchnic venous thrombosis.”
American Society of Hematology: “Blood Clots.”
CDC: “Venous Thromboembolism (Blood Clots).”
Circulation: “Postthrombotic Syndrome.”
Merck Manual Consumer Version: “Renal Vein Thrombosis,” “Portal Vein Thrombosis,” “Fainting.”
RadiologyInfo.Org: “Blood Clots.”
Blood Clot in Foot – Symptoms & Treatment


If you or someone you love suspects a blood clot, seek medical attention right away. The longer you wait, the higher your chance of developing a highly dangerous clot in one of your organs. Visit your doctor or go straight to the emergency room immediately. Clots can be life-threatening. You will want the peace of mind of a proper diagnosis. Your doctor may prescribe a blood thinner and monitor the clot. Surgery or the direct application of a clot-busting drug via a thin tube to the site of the clot may be needed. Clots are a dangerous condition that can travel through the circulatory system to anyplace in your body. If left untreated, they can become deadly. You won’t know for sure if you have one without undergoing a proper examination by a healthcare professional.
If you are experiencing any of the following symptoms, go straight to the hospital:
- Trouble breathing
- Chest pain
- Vomiting up blood
- Blood in your stool
- Dark foul-smelling stool
- Fainting spells
- Pain of numbness radiating into the left arm
- Slurred speech
- Droopy face
- Seizures
- Quick-onset confusion
What can I do to prevent a blood clot from forming?
You can take action to lower your odds of developing a blood clot. Follow a healthy diet low in fat, maintain a healthy weight, don’t smoke, and exercise regularly.
You should also:
- Avoid sitting for a long period of time, especially during a long flight or after surgery.
- If you have a desk job, set your alarm to remind you to get up and move at least every two or three hours. While sitting, flex the muscles in your legs, feet, and toes.
- Talk to your doctor about tight-fitting compression socks or garments. They may be able to help regular blood flow.
- Make an appointment with your healthcare provider. He or she may recommend taking a clot-fighting blood-thinner, sometimes called anticoagulants.
What is May-Thurner Syndrome?
May-Thurner syndrome (MTS) is a medical condition that increases one’s chances of developing blood clots. Also known as Iliac Vein Compression Syndrome, MTS occurs when the right iliac artery presses against the left iliac vein pinching the vein. This compression can cause damage to the vein and increase the risk of developing deep vein thrombosis (DVT) in the left leg. DVT is characterised by a potentially dangerous blood clot in the left leg. The clot can completely or partially block proper blood flow through the vein.
What are the warning signs for May-Thurner Syndrome?
Warning signs for MTS are subtle and very often go unnoticed. Because of this, most people do not realize they have MTS until a DVT presents itself. Individuals who experience symptoms should seek treatment. Symptoms include:
- discoloration (red or purple) of the skin,
- enlarged veins in the leg,
- leg is warm to the touch,
- swelling,
- tenderness or
- pain in the leg.
While the condition of DVT alone isn’t life-threatening, if the blood clot breaks free it has the potential to travel through the bloodstream and become lodged in the blood vessels of the lung (known as a pulmonary embolism). This is a serious and life-threatening condition.
DVT can also lead to pulmonary condition in the legs called post-thrombotic syndrome (also known as chronic venous insufficiency link). Post-thrombotic syndrome is characterized by:
- a pooling of blood in the leg,
- chronic leg swelling,
- increased pigmentation or discoloration of the skin,
- increased pressure and
- leg ulcers (known as venous stasis ulcers.)
I’ve never heard of May-Thurner Syndrome. What is it?
May-Thurner syndrome is rare. It is a vascular disorder that affects a vein in your pelvis. The right iliac artery presses against the left iliac vein, causing it to restrict blood flow. This is the vein that returns blood from your pelvis and legs back to your heart. The added pressure of the vessels pressing against each other will can cause one or both of them to narrow, impeding the blood from flowing properly. It may also cause scarring leading to a thickening of the wall. The constricted flow of blood in the leg can cause a variety of other symptoms and conditions in your legs or feet. The most problematic is perhaps a blood clot. Many people with from May-Thurner syndrome will go years without symptoms or a proper diagnosis. Over time May-Thurner syndrome can lead to:
- Swelling in the leg.
- Chronic venous insufficiency (CVI). CVI is a condition where the blood will pool within your veins, causing pressure, swelling, skin changes and venous ulcers or sores that will not heal on their own.
- Deep vein thrombosis (DVT). DVT is a blood clot in that occurs in a vein located deep below your skin. If a DVT breaks loose a moves to your lung, heart or brain it can lead to life-threatening emergencies. For example: a heart attack, stroke or a pulmonary embolism (a blood clot in your lung)
How will I know if I have May-Thurner syndrome?

Symptoms of May-Thurner syndrome can include:
- Swelling, heaviness, or a feeling of fullness in your leg or foot.
- Sores or venous ulcers on your legs or feet that don’t heal by themselves.
- Newly appearing varicose veins in your legs.
In many cases, patients have no symptoms and can go undiagnosed for years. Only when a deep vein thrombosis (DVT) develops, do many become aware of their condition.
Some symptoms of deep vein thrombosis (DVT) are:
- Swelling in the leg(s).
- Pain and/or tenderness in the leg(s).
- Changes in skin color (such as redness).
- Skin that is warm to the touch.
What are the common treatments for May-Thurner Syndrome?
You don’t have to live with the worries or symptoms of May-Thurner syndrome. It is treatable. After considering your symptoms and risk factors your healthcare provider will design a tailor-made treatment program. Any successful treatment program will effectively treat your condition while considering your lifestyle and overall health.
Common treatments for May-Thurner syndrome may include:
- Taking blood thinners or anticoagulants. These medications can help prevent blood clots.
- Thrombolysis is an intravenous procedure that we use on larger clots. In it, a catheter is feed to the site of the clot, delivering high potency anti-clotting drugs directly to the blockage. We also refer to this as “clot busting.”
- A stent is a small tube made of metal mesh that is used to hold your vein open and restore proper blood flow.
- Compression stockings are tight-fitting stocking that can ease swelling in your leg. These snug stockings are worn over your legs from your toes to knee. They apply constant pressure to your lower legs. Putting continual pressure on the area, will improve swelling and increase blood flow.
Your doctor may suggest surgery in some cases. In certain cases, surgery can be beneficial in relieving the symptoms or reducing the risks of complicating conditions brought on my blood clots. Different surgerys can be used to:
- Circumvent the section of the vein where the clot or other circumstance that is causing reduced blood flow. In this procedure, a vein is taken from another place in the body and used as a bypass, opening up the flow of blood.
- Relocate the right iliac artery. Repositioning the artery so that it is no longer pressing on the left iliac vein can open up the blood flow.
- A stent may be placed in the vein to hold it open.
What are venous ulcers?
Venous ulcers are painful sores that occur on the lower leg or around the ankle. Sometimes called venous stasis ulcers or non healing wounds, venous ulcers are lingering open wounds that don’t heal easily on their own. They frequently take, weeks, months or even longer to heal.
What are the risk factors of venous ulcers?
Various medical conditions can lead to the persistent venous ulcers. Painful venous ulcers can present themselves if you suffer from:
- Obesity
- Certain groups of medicine
- Venous insufficiency
- Diabetes
- Infections
- Venous hypertension
- Inflammatory diseases
- Kidneys failure
- Poor circulation and/or blood clots
- Varicose veins
How did I know if I have venous ulcers?

If you are at risk for venous ulcers keep an eye out for the following signs and symptoms:
- Area around the sores might be shiny. The skin may be tight and warm (or hot) to the touch.
- Discolored skin (red, purple)
- Dull ache in the leg or calf.
- Feeling of fullness or heaviness in the leg or calf.
- Swelling and cramping in the legs.
- Symptoms of blood pooling in the legs (purple, dark red, and/or brown spots. Swollen, hardened skin.)
- The edges of the ulcers are often unevenly shaped.
- Tingling and itchiness in the lower leg and/or ankle,
Stasis Ulcers: What are they?
Most commonly found on the ankle or calf, painful venous stasis ulcers are open sores that do not heal well on their own. They are typically red in color however a fibrous yellow tissue may cover them. The sores border is typically irregular. Red, purple, and brown spots may also be present on the lower legs and ankles. When suffering from venous stasis ulcers you may experience discharge and drainage. Venous stasis ulcers are common in people who have previously suffered from swollen legs and varicose veins.
Diagnosing and Treating Venous Ulcers
While diagnosing the venous ulcers is not difficult, finding the proper cause of these painful sores can be challenging. Some Western Pennsylvania providers use a duplex ultrasound. This is a noninvasive imaging test that we use to diagnose which veins are causing the venous ulcers. The difference in this approach is that it pinpoints the abnormal vein or veins. By finding the cause of the ulceration, we can treat the venous pathology and thereby prevent the return of the ulcers once healed.
After your veins have been evaluated, your healthcare provider will recommend a personalized treatment plan based on your specific needs:
 Compression Stockings for blood clot
Compression Stockings for blood clot
-
-
- Placing the leg under constant compression is a vital aspect to healing venous ulcers.
- While, compression stockings are the most commonly used tool for this treatment, there are other methods available.
- The inward compression from the stocking will counteract the pressure from the veins of the leg and allows skin to heal.
Growth factors
- Still in the testing phase, we can apply some medications to the wound. The hope is that these medicines will promote the growth of new tissue.
Hydrocolloid dressings
- Hydrocolloid dressings is specially designed dressing that is applied over the venous ulcer.
- It promotes healing and also helps to remove any debridement (non-living tissue) from the wound.
Surgery
- Sometimes you need a minor surgery to clean the wound from non-living material. Wound debridement, as it is know, removes any non-living tissue that could keep a wound from properly healing.
Transparent dressings
- We can apply a specialized clear plastic film over the wound. The pressure from the dressing, facilitates proper blood flow.
- You should wear support stockings over the wrap to hold it securely.
Unna boots
- Similar to a cast, we can custom fit a hard boot to your lower leg. Your physician will wrap a moist gauze around your lower leg (starting at the base of the toes and going to just below the knee.)
- With time, the gauze hardens and forms a snug boot around your leg.
- The boot provides additional support for the leg, improving the blood flow in your veins, healing the ulcer more quickly.
Vein Ablation for preventing a blood clot

- Vein ablation is a nonsurgical technique used to close open veins.
-






