Many readers are interested in the right subject: CPAP versus bipap-what’s the difference? We are pleased that our manufacturers have already studied the current research on this fascinating subject. We will give you a broad answer based on information from the latest medical reports, advanced research papers, and sample surveys. Keep repeating to find out more.
Since PAP devices are only available by prescription, any decision regarding the use of BIPAP, CPAP, or another form of o ridge therapy should be taken by a physician or sleep specialist.
BIPAP vs. CPAP
Update the memo periodically to expand coverage and add new information according to the latest research.
Updated December 13, 2022.
Both BIPAP and CPAP are considered types of appliances with positive breathing pressure (o ridge) that can be used to cure sleep apnea. This is a condition characterized by interrupted or weak breathing during sleep.PAP devices work by maneuvering a sleeve into a mask that is worn over the face and into the air. This air keeps the airways open and helps restore breathing during sleep.
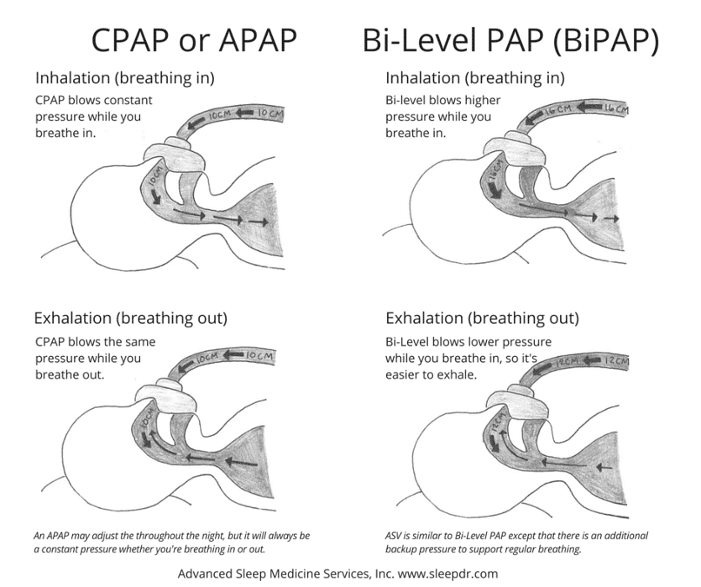
Different Pap machines work in different ways. differently CPAP machines (continuous positive airway pressure) provide constant air pressure. Bi-level positive airway pressure (BIPAP or BPAP) machines release air at a constant air pressure level. two different pressure level, one time to breathe, one time to breathe.
CPAP is generally considered the first treatment for obstructive sleep apnea (OSA), which is considered the most common form of sleep apnea; BIPAP can be prescribed for certain people who have OSA, central sleep apnea, or other breathing problems related to sleep apnea.
For people with sleep apnea, nighttime use of O-RIDGE can improve breathing and sleep; if you know what differentiates BIPAP from CPAP devices, you will better understand these treatment options and know how to best use PAP therapy.
what is bipap?
BIPAP means double positive airway pressure; a BIPAP machine guarantees air under pressure. It has the power to enclose an unclosed, non-energetic airway. This machine image can be prescribed for people with sleep-related respiratory disorders such as sleep apnea.
In contrast to CPAP machines, which usually call for air in one press, the Bippositive Machine delivers air two different Level of air pressure, breathe once, breathe once
How does Bipap work?
BIPAP works by controlling the air under pressure in the upper airway. This weightless flow prevents obstruction of the airway preventing respiratory arrest, snoring, and sleep disturbances.
The BIPAP process is ensured by introducing the machine into the bed. This is usually small enough to fit in a shoebox. The device puts air under pressure and pumps it through a connected hose. At the other end of the snake is a face mask that runs over the nose or nose and mouth. Air flows through the hose and the mask in the upper airway so breathing is not severe.
Once the BIPAP device is integrated, air is released two different Pressure Levels. Inhaled positive airway pressure (IPAP) refers to the pressure level supplied when the sleeper is inhaled. Primed positive airway pressure (EPAP) refers to the air pressure level provided when the sleeper is dried.
BIPAP machines typically guarantee more higher air pressure while the sleeper is being infiltrated and the sleeper is being sucked in and the air pressure is being lowered. The choice of air pressure is carefully calibrated to try to be as effective as possible in unraveling respiratory disorders.
How are pressure values calibrated in BIPAP?
Experts recommend implementing the BIPAP option during sleep studies in special sleep labs. During the study, the technician has the opportunity to carefully observe breathing, air values, and brain activity. With the help of this data, it can be determined which bipap pressure values have the most effect on a particular person’s breathing and sleep quality.
In addition, some BIPAP devices have integrated detectors designed to adjust the pressure value itself to prevent airway compromise. These machines can also be used to determine initial pressure values. Nevertheless, experts advise to first determine the appropriate pressure value with a sleep test.
When using a self-regulating BIPAP to determine air pressure values, physicians often examine the device’s data carefully and may recommend further sleep tests to prove that it works.
Permanent and Self-Regulating BIPAPs
There are two types of bipap devices, the image of the napping device affects the air pressure obtained during sleep
- Fixed bipap: In these devices, two fixed air pressure values (one for breathing and one for exhalation) are oriented by the physician and programmed in the device. These two values do not change during the night.
- BIPAP Self-Regulation. BIPAP devices with self-regulation have the option to adjust pressure values to sleeper breaths. However, these BIPAP devices start with pre-programmed basic pressure values for inhalation and exhalation and use detectors to predict how to breathe and adjust pressure values as needed.
Because self-applied BIPAP devices are considered more recent, there is limited data showing that they treat sleep apnea and other breathing difficulties in the same way as fixed BIPAP devices.
What are the different treatment modalities of BIPAP?
The BIPAP device can be programmed to operate in one of three positions. different The mode depends on what is needed to solve the breathing problem.
- Spontaneous mode: In spontaneous mode, the machine delivers only choked air while it detects that the person begins to come in and out.
- Timed mode (T): In timed mode, the machine delivers air according to a preset timer, not according to breathing.
- Spontaneous Time Mode (S/T): In this mode, the BIPAP device drives air when the sleeper begins to breathe. However, there is also a timer that activates the device to deliver air if the sleeper does not breathe for a period of time.
What are the superior qualities of BIPAP?
The use of PAP therapy is very advantageous for those with obstructive sleep apnea by reducing daytime sleepiness and improving well-being and overall quality of life. For people with obstructive sleep apnea, the most important advantage of BIPAP is that it is more comfortable to use than CPAP devices because of the lower air pressure produced during exhalation.
People who require higher air pressure during breathing to eliminate sleep apnea symptoms may benefit from BIPAP. It is difficult to tolerate higher air pressure while exhaling. By providing lower pressure while exhaling, the BIPAP device can begin to run at night. This is essential in the treatment of sleep apnea.
Because the BIPAP device can be programmed with timer support, BIPAP therapy remains helpful for those with illnesses that cause slow, irregular breathing, including central sleep apnea. In these cases, BIPAP helps regulate breathing and sleep better.
What are the defects of Bipap?
The most important problem with using BIPAP for obstructive sleep apnea is that the pressure may be inadequate and the cost may be high.
The BIPAP system lowers the air pressure during exhalation. For some people, the pressure could be very low to keep the airway open and safely treat obstructive sleep apnea.
Another possible flaw is that BIPAP devices can be more expensive than CPAP devices. Those who are insured for the device may not be aware of the huge price tag. difference However, BIPAP therapy could have a significant financial impact on those who have to pay for the device out of their own pockets.
how does bipap bounce from cpap?
The key difference between bipap and cpap differ from each other because the bipap device provides different air pressure levels during inhalation and exhalation. cpap machines use the same air pressure, regardless of whether the sleeper using the machine or not.
However, in many respects the differences between BIPAP and CPAP devices are getting smaller and smaller. It is not uncommon for a modern CPAP device to warrant more than one air pressure setting. For example, the pressure reduction setting of many CPAP devices ensures that the air pressure is less noticeable during breathing.
is bipap better than cpap?
Studies have shown similar results with both CPAP and BIPAP in treating obstructive sleep apnea (OSA); most people with OSAS are initially recommended for CPAP because of its simplicity and ease of use. However, there are situations in which BIPAP therapy is more effective than CPAP.
Who is best suited for BIPAP?
The BIPAP device is generally best suited for individuals who have difficulty in getting to sleep or who have difficulty with CPAP therapy.
It is most often used in two specific cases in people who have obstructive sleep apnea problems and no other sleep breathing problems
- When higher pressure is needed: significantly higher air pressure is needed during breathing to prevent breathing problems; the BIPAP device ensures higher air pressure and then lowers the pressure during exhalation.
- If initial CPAP therapy is ineffective: while CPAP can help almost all people with obstructive sleep apnea, it is not effective for everyone. Additionally, some people are concerned about the air pressure that the CPAP device produces when they breathe in. In these cases, switching to BIPAP therapy can help improve breathing during sleep.
BIPAP is often considered the best treatment option for those suffering from complex respiratory disorders that occur simultaneously with obstructive sleep apnea.
For example, BIPAP therapy may be prescribed for people with certain forms of central sleep apnea (CSA). This is caused by faulty signals to the brain and muscles that control breathing. between It is caused by faulty signals to the brain and muscles that control breathing. In particular, BIPAP is often well recommended for people with CSA associated with welfare challenges with any chance of causing slower and fewer breaths, including
- Muscular dystrophy
- Obesity Hypoventilation Syndrome (OHS)
- Chronic obstructive pulmonary disease (COPD)
- Customary use of opioid medications
Since PAP devices are only available by prescription, any decision regarding the use of BIPAP, CPAP, or another form of o ridge therapy should be taken by a physician or sleep specialist.
How Do I Maximize BIPAP Therapy?
To maximize BIPAP therapy, you should follow all the instructions of your physician or sleep specialist. For example, your physician can offer advice on the possibilities of the BIPAP device, how often to use the device, and how to use it clean. It is also advisable to go through the various maintenance leaflets of the device manufacturer.
The use of a mask that fits well and prevents air leakage remains essential for successful polydge therapy. It is advisable to try several masks before finding the best one, so if the first mask feels uncomfortable or leaks air, consult your doctor.
Consult your own physician or sleep specialist if you experience problems with your BIPAP vehicle, with your mask or other device, or if you experience breathing problems or other symptoms.
When looking at other ventilators
While BIPAP devices may be helpful in many life conditions, there are times when you may need to consider other ventilators.
For example, if you have obstructive sleep apnea without other breathing problems, a CPAP machine may be recommended to begin treatment; BIPAP therapy is not yet appropriate for people with central sleep apnea or certain health problems, including certain types of heart failure.
If you have already started using a BIPAP machine and there is no improvement in your symptoms, you may want to take another picture of your ventilator. If there have been recent changes in symptoms or general health, the healing project can be adjusted.
Frequently Asked Questions about BIPAP and CPAP
How does BIPAP differ from APAP?
Self-adaptive positive airway pressure devices (APAPs) function similarly to CPAP devices, but change the air pressure supplied in response to breathing patterns. Self-adaptive development is still built into BIPAP devices, but BIPAP is often prescribed with a fixed air pressure option.
APAP devices remain popular as autoclaves and can be used as initial treatment for people with obstructive sleep apnea who do not have other respiratory disorders or problems. Typically, BIPAP devices are not prescribed for obstructive sleep apnea in the first instance. Instead, BIPAP therapy is often tried when a person with OSA cannot tolerate CPAP or APAP therapy.
Is BIPAP more valuable than CPAP?
In most cases, BIPAP devices cost more than CPAP devices. At the very least, the actual price out of your own pocket will depend on your health insurance.
Are BIPAP machines more CPAP?
While there may be some differences based on brand and model, most BIPAP and CPAP devices are about the same size. These devices usually fit well on a bedside table and are easy to reach at night.
Do I need a recipe for my BIPAP device?
To get a Bipon device or another ridge-like therapy, you need a recipe. Therefore, it is essential to speak with your doctor or sleep specialist about your breathing dilemma during sleep.
Is the pressure increase feature available in BIPAP devices?
Many BIPAP devices have a pressure increasing function. The disaster function ensures that the air pressure is low during the first 5-45 minutes of use. The device will then start chatting at the full pressure specified.
How do you know if Bipap works?
The effectiveness of BIPAP therapy is determined by following changes in symptoms and testing the information registered by the device. the BIPAP device collects data on breathing during sleep, and the physician can view this data to see how BIPAP improves breathing difficulties. The BIPAP device collects data on breathing during sleep.
Recommendations
- Consulted on August 14, 2022.
- Consulted on August 14, 2022.
- Consulted on August 14, 2022.
- Consulted on August 14, 2022. https: // PubMed. NCBI. NLM. NIH (National Institutes of Health. Gov/30736887/
- Accessed August 14, 2022.
- Accessed August 14, 2022.
- Accessed August 14, 2022. https://www. ncbi. nlm. nih. gov/books/nbk459252/.
- Accessed August 14, 2022.
- Accessed August 14, 2022.
- Accessed August 14, 2022.
- Accessed August 14, 2022. https://pubmed. ncbi. nlm. nih. gov/30736888/
- Accessed August 14, 2022.
- Accessed August 14, 2022.
- Accessed August 14, 2022.
- Accessed August 14, 2022.
- Accessed August 14, 2022 Accessed August 14, 2022 Accessed August 14, 2022
- Accessed August 14, 2022 Accessed August 14, 2022 Accessed August 14, 2022 Accessed August 14, 2022
- Accessed August 14, 2022 Accessed August 14, 2022 Accessed August 14, 2022 Accessed August 14, 2022
- Accessed August 14, 2022 Accessed August 14, 2022 Accessed August 14, 2022 Accessed August 14, 2022
- Accessed August 14, 2022.
About the Author
Fiction Employee, Product Testing Team
Allison is a healthcare writer with the skills necessary to read and interpret peer-reviewed academic research. Based in San Diego, she has published articles in the journals PLOS Genetics and Journal of BioChemistry and is a staff writer for SmartBug Media. She holds a master’s degree in biochemistry from the University of California, Davis, and has nearly a decade of experience in life science research. She enjoys helping people ignore the noise and understand the bigger picture of sleep and health. Allison likes to stay busy climbing, hiking, and walking with her dog.
Ask Sleep Doctor
If you have questions, send an electric message to the Sleep Doctor team. Not only can we give you the answers you need, we can also help you get to sleep.
CPAP Vs. BIPAP-What is the difference and how do they relate to each other?


CPAP Vs. BIPAP-What is it? the differences What Do You Need?
Sleep apnea is considered a simple sleep disorder in which breathing repeatedly goes in and out. People with sleep apnea usually have headaches and irritability that persist in the morning, even after a full night’s sleep.
Sleep apnea is one of the most common sleep disorders because it affects 3% to 7% of the population. However, this condition can be a life-changing problem for those who have it. There are healing options that can help. However, there are CPAP cushions and other forms of sleep medicine that can help. The more well-known options for healing sleep apnea are CPAP therapy and BIPAP.
Continuous positive airway pressure (CPAP) is considered the more common porridge treatment, while bilevel positive airway pressure (BIPAP) is more common for others. However, both work equally well. key differences between 2 that determine their effectiveness for a particular condition. Finally, what is the differences between CPAP versus BIPAP and how do they relate to each other?
What is the difference between CPAP and BIPAP devices?
CPAP and BIPAP devices also work in similar ways, but they treat different types of sleep apnea. There are three types of sleep apnea: obstructive sleep apnea, central sleep apnea, and mixed sleep apnea. Each of these forms, such as obstructive sleep apnea and central sleep apnea, is important to know because they likely affect well the difference between BIPAP versus CPAP machine, so you can know what the best option is in your case.
The difference between CPAP machines and BIPAP machines can be attributed to the number of pressure options that both guarantee.
– With CPAP machines (continuous airway pressure), the patient receives a single pressure from an endless flow of air through the face mask.
The BIPAP device, on the other hand, offers two pressure options.
– One for inhalation and a lower pressure for exhalation. This is why almost all patients with sleep apnea feel more comfortable with BIPAP, as it can better adapt to their needs.
With CPAP and BIPAP machines, the airway is pressed against the air under pressure from the machine so that the patient can breathe through the night each day. if CPAP therapy is unacceptable, BIPAP therapy enters the picture with two pressure variations that guarantee.
For both CPAP machines and beepers, it is essential to keep the mask and hose clean during use. This can be done with the help of CPAP cleaner or soap intended for mask cleaning.
To switch from a CPAP device to a BIPAP device, medical advice should be obtained from a physician so that the patient can authorize the switch. between These machines are covered by insurance.
CPAP Explained.

A continuous positive airway pressure machine guarantees the full pressure of an endless weightless jet through a full face mask that the patient wears while sleeping to support breathing. The machine guarantees and is said to be used also to cure other signs that breathing is broken, snoring occurs, and with that amount of position.
- Increased daytime sleepiness
- Insomnia
- Nightmares
- Dry mouth
- Headaches
- Irritability
CPAP devices are equipped with adjustable pressure settings that vary from 4 to 20 cm H2O while the user breathes. frequent medical uses of CPAP machines are for the treatment of obstructive sleep apnea (OSA) and the use of the machines in premature infants.
Obstructive sleep apnea has a significant impact on mental and vascular function and is associated with disorders such as congestive heart failure and hypertension. This condition can still overlap with late-stage obstructive pulmonary disease (COPD) and can cause long-term health problems.
To determine the non-weight jet pressure needed to cure sleep apnea, you should consult your own physician so that he or she can make an estimate based on your needs. This is usually based on anatomy or weight or on a more thorough look at the situation using a sleep test.
People with sleep apnea are usually started on a CPAP device. This condition is often caused by someone who has had a cardiac arrest or heart attack or who has used narcotics.
Bipap explained

BIPAP therapy (positive air pressure) includes two air pressure options that the device can change between while the patient breathes at night. With all pressure devices, the patient has every opportunity to change between higher pressure and breathe at a higher pressure and breathe at a slightly lower pressure with the absolute face mask. Most BIPAP devices have a spectrum of 4 to 25 cm H2O, 5 cm higher than CPAP devices.
The two air pressure options displayed on the BIPAP device are a higher inlet pressure called IPAP and a lower formula called EPAP. the BIPAP device itself contains up to three switching options between IPAP and EPAP:
The first air pressure setting on the BIPAP device is a short-term switching setting that allows the user to set how long the IPAP and EPAP pressures will last. This adjustable feature allows the user to create the correct number of breaths per minute to obtain the next cure for the condition.
Second, the device has a spontaneous switching property that senses the user’s breathing pattern, switching between between IPAP and EPAP air pressure settings. This setting is considered normal for a BIPAP machine, for example, because this setting is related to the night’s sleep measured.
Spontaneous/ Time combines the first two options, including finally the switching time when the device detects that the user’s breathing corresponds to a set number of breaths per minute. This advanced agency follows the user’s natural breathing pattern.
bipap vs. cpap: which is better than the other?
To make the best choice for your condition, you need to examine BIPAP therapy compared to CPAP the difference between ii. With continuous positive airway pressure therapy (CPAP), the machine is used to cure obstructive sleep apnea (OSA). It supports the patient’s airway and helps him or her breathe more during sleep than normal. Obstructive sleep apnea is considered the most common form of this condition.
BIPAP devices are often used to treat central sleep apnea (CSA) and obstructive sleep apnea, as well as cardiac, non-spinal, and neurological disorders that urgently ask the patient to prompt structured breathing during sleep. Treatment of difficult forms of sleep apnea with the help of sleep medicine and a Bepod or CPAP device is important to prevent long-term effects on your well-being.
Typically, people with sleep apnea and other sleep disorders begin with a CPAP machine for curative therapy. When a patient uses a CPAP machine with a CPAP mask for the first time, there is usually an adjustment phase before the patient becomes accustomed to the support of the device.
If the patient experiences discomfort with CPAP therapy, adjust and tune the pressure options, different type of mask and to try the climate control device for those who have been conditioned to the option.
If you are trying to use continuous positive airway pressure to treat sleep apnea and find that CPAP therapy is not right for you, it is important to talk to your doctor about switching from CPAP to BIPAP therapy. This switch between The choice of these pressure devices must be approved by your physician and should be accompanied by a sleep specialist to ensure that the switch is appropriate for your healing.
If you believe you have sleep apnea, contact your own physician. Your physician can further evaluate your condition and possibly refer you to a sleep specialist for a sleep study. The device must then be approved by your sleep specialist or physician in order to be covered by your insurance. Untreated sleep apnea can increase the risk of serious health problems, so it is important to detect the condition as soon as possible.
Conclusion CPAP and BIPAP (most important characteristics and differences):
CIPAP
- Continuous
- Equal pressure for exhalation and inhalation
- Used at home
- Usually complex device
- Requires little control
- Cheaper than BIPAP
BIPAP
- Continuous
- Pressures are different between Inhalation and exhalation (exhalation 5 cm aquacolom inhalation opposite 15 cm aquacolom)
- Not often used in family situations
- No simple device
- Need to check blood pressure
- Interval






